MOVEMENT IS MEDICINE, ADD LIFE TO YEARS!
Physiotherapy: Where ART meets SCIENCE
Physiotherapy, often perceived as a blend of medical science and therapeutic artistry, is a holistic discipline dedicated to enhancing and restoring physical function and mobility. This field goes beyond the mere application of techniques; it embodies the art of understanding the human body and the science of healing.
Explore our advanced physiotherapy, chiropractic clinic & neurorehab centre for comprehensive rehab services.


NEUROLOGICAL REHABILITATION: Comprehensive Assessment, Screening, and Management
Neurological rehabilitation is a specialized field within physiotherapy focused on improving the functional abilities and quality of life for individuals with neurological conditions such as stroke, multiple sclerosis, Parkinson’s disease, traumatic brain injury, and spinal cord injuries. This multifaceted approach encompasses thorough assessment, meticulous screening, and personalized management strategies.
Assessment and Screening
The cornerstone of effective neurological rehabilitation is a detailed assessment. This process begins with a comprehensive patient history, understanding the onset, duration, and progression of symptoms. Neurological examinations include:
1. Motor Function Assessment: Evaluates muscle strength, tone, and movement patterns.
2. Sensory Testing: Assesses sensation, proprioception, and pain perception.
3. Cognitive and Psychological Screening: Identifies issues related to memory, attention, mood, and behavior.
4. Functional Assessments: Measures activities of daily living (ADLs), mobility, and independence levels.
5. Balance and Gait Analysis: Utilizes tools like the Berg Balance Scale, Timed Up and Go Test, and observational gait analysis to assess stability and walking patterns.
Management Strategies
Based on the assessment, a tailored rehabilitation plan is developed. Key components include:
1. Balance Training: Essential for preventing falls and enhancing stability. Interventions may involve static and dynamic exercises, such as standing on varied surfaces, using balance boards, and practicing weight shifts. Virtual reality and biofeedback can also be utilized to provide real-time feedback and engage patients in interactive balance tasks.
2. Gait Training: Focuses on improving walking ability, often compromised in neurological conditions. Techniques include treadmill training, overground walking, and the use of assistive devices like canes or walkers. Advanced methods may incorporate robotic-assisted gait devices and functional electrical stimulation (FES) to stimulate muscle contractions and enhance walking patterns.
3. Coordination Exercises: Target the fine-tuning of motor skills. Activities might include practicing hand-eye coordination tasks, using therapy balls, or performing targeted exercises to improve limb control and accuracy. Repetitive and task-specific training helps in re-establishing neural pathways and improving motor coordination.
4. Functional Training: Aims at enhancing the ability to perform everyday tasks. This includes exercises to improve strength, endurance, and flexibility. Functional electrical stimulation (FES) can be used to activate muscles during activities, promoting more efficient and effective movement patterns. Occupational therapy may be integrated to focus on specific ADLs, such as dressing, cooking, and personal hygiene.
5. Neuroplasticity and Task-Specific Training: Leveraging the brain’s ability to reorganize itself by forming new neural connections. Intensive, repetitive, and task-specific training helps in recovering lost functions. Techniques like constraint-induced movement therapy (CIMT) for upper limb recovery and body-weight supported treadmill training (BWSTT) for gait recovery are commonly used.
ORTHOPAEDIC REHABILITATION: Comprehensive Assessment and Targeted Management


Orthopaedic rehabilitation is a vital branch of physiotherapy dedicated to the assessment, treatment, and prevention of musculoskeletal disorders. It addresses issues related to bones, joints, muscles, tendons, and ligaments, aiming to restore optimal function and alleviate pain. Conditions commonly managed include fractures, post-surgical recovery, arthritis, sports injuries, and chronic musculoskeletal pain.
Assessment and Screening -
Effective orthopaedic rehabilitation begins with a thorough assessment to identify the root cause of the dysfunction and to formulate a tailored treatment plan. Key components of the assessment include:
1. Patient History: Collecting detailed information about the onset, nature, and duration of symptoms, as well as previous injuries or surgeries.
2. Physical Examination: Evaluating posture, gait, and functional movements. Palpation, range of motion (ROM) testing, and muscle strength assessments are critical to identify areas of restriction and weakness.
3. Diagnostic Tests: Utilizing imaging studies (e.g., X-rays, MRIs, CT scans) and special orthopedic tests (e.g., Lachman test for ACL integrity, Neer’s test for shoulder impingement) to further pinpoint the diagnosis.
4. Functional Assessments: Measuring the patient’s ability to perform activities of daily living (ADLs) and specific tasks related to their lifestyle or occupation.
Management Strategies -
Based on the comprehensive assessment, a personalized rehabilitation plan is developed, focusing on pain relief, restoration of function, and prevention of further injury. Key management strategies include:
1. Pain Management: Initial stages often involve modalities such as ice, heat, ultrasound, and electrical stimulation (e.g., TENS) to alleviate pain and reduce inflammation. Manual therapy techniques, including joint mobilizations and soft tissue massage, are also employed to ease discomfort.
2. Range of Motion (ROM) Exercises: Restoring flexibility and joint mobility through passive, active-assistive, and active stretching exercises. Techniques such as proprioceptive neuromuscular facilitation (PNF) stretching are effective in improving ROM.
3. Strengthening Exercises: Focused on rebuilding muscle strength and endurance. Progressive resistance exercises using weights, resistance bands, and body-weight activities are tailored to the specific needs of the patient. Eccentric exercises are particularly beneficial for tendinopathies.
4. Functional Training: Emphasizes the restoration of functional abilities necessary for daily activities and work-related tasks. This includes task-specific exercises, balance training, and proprioceptive activities to enhance coordination and stability.
5. Gait and Posture Correction: Addressing abnormalities in walking patterns and posture that may contribute to pain or dysfunction. Techniques such as gait re-education, postural training, and the use of orthotic devices (e.g., insoles, braces) are employed to correct these issues.
6. Post-Surgical Rehabilitation: Structured programs designed to promote healing, regain function, and prevent complications following orthopedic surgeries such as joint replacements, ligament repairs, and fracture fixations. Emphasis is placed on controlled mobilization, strengthening, and gradual return to normal activities.
7. Education and Prevention: Educating patients about their condition, proper body mechanics, ergonomic principles, and injury prevention strategies. This empowers them to manage their health proactively and avoid re-injury.
SPORTS REHABILITATION: Optimizing Recovery and Performance


Sports rehabilitation is a specialized branch of physiotherapy focused on helping athletes recover from injuries, improve performance, and prevent future injuries. This field combines evidence-based practices with sport-specific knowledge to ensure athletes return to their sport safely and at peak performance. Key elements of sports rehabilitation include comprehensive assessment, targeted intervention, and ongoing management tailored to the unique demands of athletic activities.
Assessment and Screening -
A thorough assessment is crucial to identify the extent of the injury, understand the underlying causes, and develop an individualized rehabilitation plan. This process involves:
1. Injury History: Detailed documentation of the injury’s mechanism, onset, and progression, along with the athlete’s previous injury history and medical background.
2. Physical Examination: Evaluating the injured area for signs of swelling, bruising, deformity, and tenderness. Assessing joint range of motion (ROM), muscle strength, and functional capabilities.
3. Functional Movement Screening: Utilizing standardized tests (e.g., Functional Movement Screen) to identify movement deficiencies and imbalances that may contribute to the injury or affect performance.
4. Diagnostic Imaging: When necessary, incorporating X-rays, MRIs, or ultrasounds to obtain a precise understanding of the injury’s severity and structure involved.
Management Strategies -
Based on the assessment, a tailored rehabilitation plan is developed to address the specific needs of the athlete and their sport. Key components include:
1. Acute Injury Management: Initially, the focus is on reducing pain and inflammation through modalities such as ice, compression, elevation, and electrical stimulation (e.g., TENS). Immobilization or bracing may be used to protect the injured area.
2. Restoring Mobility and Flexibility: Gradual progression of ROM exercises to restore joint flexibility and prevent stiffness. Techniques like passive and active stretching, proprioceptive neuromuscular facilitation (PNF), and manual therapy (e.g., joint mobilizations, soft tissue massage) are employed.
3. Strengthening and Conditioning: Tailored strength training programs targeting the injured area and overall body conditioning to ensure balanced muscle development and reduce the risk of re-injury. Progressive resistance exercises using weights, resistance bands, and body-weight activities are customized to the athlete’s needs.
4. Functional and Sport-Specific Training: Integrating exercises that mimic the demands of the athlete’s sport. This includes plyometrics, agility drills, balance training, and coordination exercises to enhance neuromuscular control and proprioception. Sport-specific drills and activities are incorporated to ensure a smooth transition back to the sport.
5. Gait and Biomechanical Analysis: Assessing and correcting gait patterns and biomechanics to address any abnormalities that may contribute to the injury or affect performance. Techniques such as video gait analysis, orthotic prescription, and biomechanical training are utilized.
6. Return to Play (RTP) Protocols: Establishing clear criteria for safe return to sport, including pain-free movement, full ROM, adequate strength, and sport-specific functional capabilities. RTP protocols often include progressive loading, monitored sport-specific drills, and simulated game scenarios to assess readiness.
7. Injury Prevention: Educating athletes on proper warm-up and cool-down routines, sport-specific conditioning, and techniques to prevent future injuries. Emphasizing the importance of rest, recovery, and balanced training to maintain long-term athletic health.
Advanced Techniques -
Innovations in sports rehabilitation include the use of advanced technologies and techniques such as:
• Cryotherapy: Utilizing cold therapy to reduce inflammation and speed up recovery.
• Kinesio Taping: Applying elastic therapeutic tape to support muscles and joints without restricting movement. To know more about Kinesio Taping, click here.
• Blood Flow Restriction (BFR) Training: Using controlled occlusion to enhance strength gains with lower intensity exercises.
POSTURE CORRECTION & ERGONOMIC ADVICE
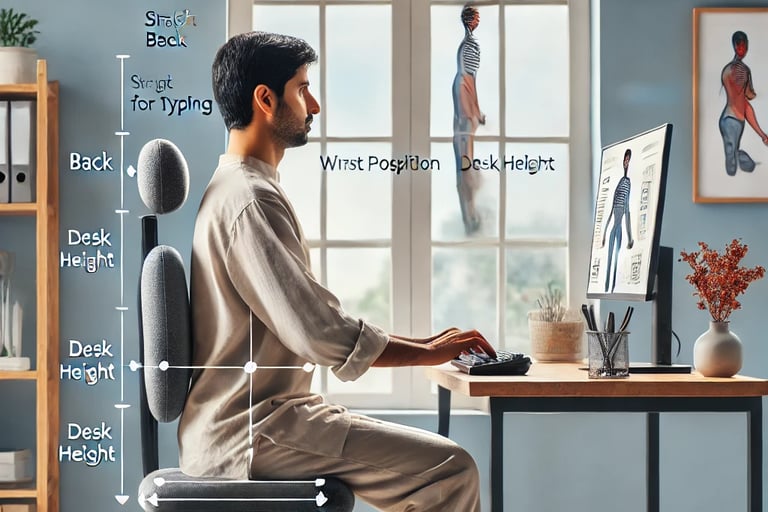
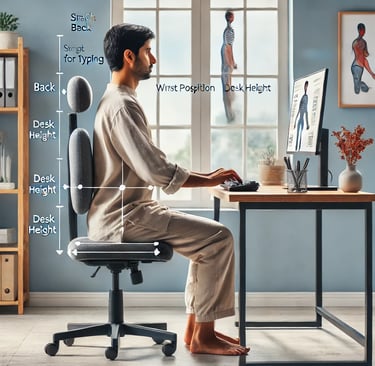
Maintaining good posture and adopting ergonomic practices are essential for preventing musculoskeletal disorders, especially for individuals who spend long hours sitting at desks or working in static positions. Proper posture not only reduces the risk of back, neck, and shoulder pain but also enhances overall physical well-being and productivity. Ergonomics involves adjusting your workstation and habits to align with the body’s natural posture, promoting comfort, and minimizing strain on muscles and joints. In the context of a modern lifestyle, where many people work remotely or spend extensive time on digital devices, posture correction and ergonomic solutions become even more crucial.
Assessment & Screening -
To ensure an effective posture correction program, the first step involves thorough assessment and screening. This process helps in identifying any existing postural imbalances, muscle weaknesses, or joint misalignments that may contribute to discomfort or long-term health issues.
Postural Evaluation: A detailed visual and physical examination to identify areas of postural deviation, such as rounded shoulders, forward head posture, or slouching. Observation of standing and sitting postures to assess any noticeable alignment issues in the spine, shoulders, hips, and neck.
Range of Motion Screening: Assessing the flexibility and movement patterns of the spine, neck, shoulders, and lower back to detect restrictions or discomfort during movement. Identifying any limited range of motion that might be contributing to poor posture or increased strain on certain muscle groups.
Muscle Strength and Endurance Testing: Checking the strength of key postural muscles, including the core, back extensors, glutes, and shoulder stabilizers. Testing for any muscle imbalances, such as overactive chest muscles and weak upper back muscles, that can affect posture.
Ergonomic Workstation Review: Analyzing the user’s workstation setup to ensure it supports good posture. This includes reviewing desk height, chair positioning, monitor placement, and keyboard/mouse ergonomics. Recommendations for proper seating, lumbar support, and adjusting workstations to reduce repetitive strain injuries and promote a neutral spine alignment.
Functional Movement Testing: Assessing common movements performed during daily activities, such as lifting, reaching, or bending, to identify improper mechanics that could lead to injury or discomfort. Screening for any compensatory movements that arise from postural misalignments.
Lifestyle and Habit Evaluation: Identifying lifestyle factors that may contribute to poor posture, such as long periods of sitting, lack of physical activity, or incorrect sleeping positions. Recommendations for habit changes and exercises that promote better posture and spinal health.
By conducting a comprehensive assessment and screening, physiotherapists can create a tailored posture correction plan that focuses on strengthening weak areas, improving flexibility, and adjusting daily habits to ensure long-term comfort and health.
Management strategies
Workstation Ergonomics:
Chair Setup: Ensure the chair provides proper support for the lower back (lumbar region). Adjust the chair height so that your feet are flat on the floor and your knees are at a 90-degree angle.
Desk Height: The desk should be at a height that allows your forearms to rest parallel to the ground with your elbows bent at about 90 degrees.
Monitor Placement: The top of the screen should be at or slightly below eye level. Maintain a distance of about an arm’s length from the monitor to reduce eye strain and neck discomfort.
Neutral Spine Alignment: Keep your spine in a neutral position when sitting or standing. Avoid slouching or leaning forward, which can lead to back and neck strain.
Shoulder Position: Keep your shoulders relaxed and avoid hunching them forward. Ensure they are aligned with your ears to reduce tension in the neck and upper back.
Foot Position: Whether sitting or standing, your feet should be flat on the floor or on a footrest, with your weight evenly distributed.
Frequent Breaks and Movement:
Take Breaks: Stand up, stretch, or walk every 30 minutes to an hour. Prolonged sitting can lead to poor posture and muscle imbalances.
Change Positions: Shift positions frequently. Alternate between sitting and standing if possible by using a sit-stand desk or by taking short walking breaks.
Strengthening and Flexibility Exercises:
Core Strengthening: A strong core supports good posture. Incorporate exercises like planks, bridges, and abdominal holds to improve core stability.
Postural Muscles: Strengthen the muscles responsible for maintaining posture, including the back, shoulders, and neck. Exercises like scapular retractions, rows, and shoulder blade squeezes can help.
Stretching: Stretch tight muscles, especially the chest, hip flexors, and hamstrings, which can contribute to poor posture.
Use of Ergonomic Aids:
Lumbar Support: Use a lumbar support cushion or a chair with built-in lower back support to maintain the natural curve of your spine.
Wrist Support: Use wrist pads while typing or ensure the keyboard is positioned to keep your wrists straight to reduce strain.
Footrests: If your feet don’t reach the ground while sitting, use a footrest to maintain proper leg positioning.
Correct Sleeping Posture:
Sleeping Position: Sleep on your back or side with a pillow that supports your neck in a neutral position. Avoid sleeping on your stomach, as it can strain the neck.
Pillow and Mattress: Use a supportive pillow and mattress that keep your spine aligned. A firmer mattress may help in maintaining spinal support during sleep.
Posture Awareness and Mindfulness:
Be Conscious of Your Posture: Regularly check in with your posture throughout the day, especially when working at a desk or standing for long periods.
Mindfulness and Relaxation: Incorporate mindfulness techniques, such as deep breathing or meditation, to reduce tension in your muscles and enhance body awareness.
Workplace Adjustments:
Tailored Ergonomics: Customize your workspace setup based on your unique needs. Adjust the chair, desk, and monitor height to fit your body dimensions.
Task-Specific Ergonomics: If your work involves repetitive tasks (e.g., typing or lifting), ensure those activities are designed to minimize strain.
Long-Term Management:
Consistency: Regularly practicing proper posture and ergonomics in daily activities is crucial for long-term results.
Ongoing Assessment: Periodically reassess your posture and workstation to make adjustments as needed, especially if you notice discomfort or new habits developing.
Education and Training: Learning about proper body mechanics, ergonomic adjustments, and postural exercises can reinforce the long-term adoption of healthy habits.
These strategies aim to improve posture, reduce pain, and prevent musculoskeletal issues through better ergonomic practices and body awareness. Consult a physiotherapist for personalised management strategies for your specific needs!
CARDIO - PULMONARY REHABILITATION


Cardiopulmonary Rehabilitation is a medically supervised program designed to improve the cardiovascular and respiratory health of individuals recovering from heart disease, lung disorders, or surgery. It combines exercise training, education, and lifestyle modifications to enhance endurance, lung capacity, and overall heart function.
Assessment & Screening -
Assessment and Screening in Cardiopulmonary Rehabilitation are essential steps to design a safe and effective rehabilitation program tailored to the individual's needs. These steps help in identifying the patient's current health status, physical abilities, and risks, ensuring the program is customized for optimal recovery.
1. Medical History Review: A comprehensive review of the patient’s medical history, including past heart or lung conditions, surgeries, medications, and any existing health problems such as diabetes, hypertension, or obesity.
2. Physical Examination: The physiotherapist or doctor conducts a physical exam, focusing on cardiovascular and respiratory function. This includes checking heart rate, blood pressure, lung sounds, and any signs of swelling or fluid retention.
3. Functional Capacity Testing: Six-Minute Walk Test (6MWT): A simple test to measure how far the patient can walk in six minutes, which helps gauge cardiovascular fitness and endurance. Treadmill or Bike Stress Test: Used to evaluate how the heart and lungs respond to increased physical activity under controlled conditions.
4. Pulmonary Function Tests (PFTs): These tests assess lung function, measuring the volume of air the patient can inhale and exhale, and how well oxygen is transferred from the lungs to the bloodstream. Spirometry is commonly used for this.
5. Electrocardiogram (ECG/EKG): An ECG is used to monitor the heart’s electrical activity, detecting any abnormal rhythms or signs of stress on the heart during rest or exercise.
6. Blood Tests: Blood tests, including cholesterol levels, blood sugar, and markers of heart damage (like troponin levels), are often checked to understand the patient's overall health and risk factors.
7. Oxygen Saturation Levels (SpO2): Monitoring oxygen levels, especially during exercise, to ensure the patient’s lungs are efficiently delivering oxygen to the blood. This can guide the use of supplemental oxygen if necessary.
8. Psychological Assessment: Anxiety, depression, and emotional stress are common among individuals recovering from heart or lung issues. Screening for mental health conditions helps address psychological barriers to recovery.
9. Risk Stratification: Patients are classified into low, moderate, or high-risk categories based on their medical history, test results, and physical condition. This determines the intensity and level of monitoring required during rehabilitation.
10. Goal Setting: After assessment, realistic short-term and long-term goals are set, such as improving exercise tolerance, reducing symptoms, and enhancing overall quality of life.
Management Strategies in Cardiopulmonary Rehabilitation -
Cardiopulmonary rehabilitation aims to improve cardiovascular and pulmonary function, enhance physical fitness, and promote long-term heart and lung health. Here are key management strategies:
1. Exercise Training -
Aerobic Exercise: Tailored activities such as walking, cycling, and swimming to improve cardiovascular endurance and oxygen utilization. Example: Start with low to moderate intensity (e.g., walking on a treadmill) for 20-30 minutes, 3-5 times a week, progressively increasing intensity as fitness improves.
Resistance Training: Strengthens muscles, reduces fatigue, and supports functional movement. Example: Light weights, resistance bands, or bodyweight exercises performed 2-3 times a week.
Breathing Exercises: Techniques such as diaphragmatic breathing and pursed-lip breathing to enhance lung function and reduce shortness of breath.
2. Lifestyle Modifications -
Smoking Cessation: Critical for lung health. Patients receive counseling or support programs to quit smoking.
Healthy Eating: Patients are educated on a heart-healthy and lung-friendly diet, including reducing sodium, cholesterol, and processed foods while increasing fruits, vegetables, and whole grains.
Weight Management: For overweight patients, a structured plan is introduced to achieve a healthy weight through a balanced diet and regular physical activity.
3. Risk Factor Control -
Blood Pressure Management: Encouraging adherence to medications, regular monitoring, and lifestyle changes to control hypertension.
Cholesterol Management: Patients are advised on diet and medications like statins to control cholesterol levels and prevent heart complications.
Blood Sugar Control: Especially for patients with diabetes, blood glucose monitoring and appropriate diet or medication plans are essential to avoid complications.
4. Medical Supervision and Monitoring -
Heart Rate and Blood Pressure Monitoring: Patients are monitored before, during, and after exercise to ensure they stay within safe limits. Heart rate targets are set based on the individual’s condition.
Oxygen Therapy: For patients with severe lung disease, supplemental oxygen may be used during exercise to maintain adequate oxygen saturation.
Continuous Evaluation: Regular assessments ensure the program is progressing safely. Adjustments are made based on the patient’s response and progress.
5. Education and Self-Management Training -
Patient Education: Regular educational sessions on topics like heart and lung anatomy, disease management, medication adherence, and lifestyle changes.
Symptom Recognition: Teaching patients to recognize warning signs (e.g., chest pain, shortness of breath) and when to seek medical help.
Medication Management: Ensuring patients understand their medications, their purpose, and the importance of adherence.
6. Psychological and Emotional Support -
Counseling: Psychological support, including therapy or counseling for anxiety, depression, or fear of exertion, which is common in patients with heart or lung disease.
Support Groups: Peer support or group sessions provide emotional support and motivation from others undergoing similar experiences.
Stress Management: Relaxation techniques such as meditation, yoga, or breathing exercises are incorporated to reduce emotional stress and improve overall well-being.
7. Long-term Maintenance Program -
Home Exercise Programs: After completing the rehabilitation program, patients are encouraged to continue exercise at home or in community settings. They receive guidance on maintaining activity levels safely.
Follow-up Appointments: Regular follow-up with the healthcare team to monitor long-term progress, adjust exercise plans, and check for any recurrence of symptoms or complications.
Behavioral Changes: Emphasis on maintaining lifestyle changes such as diet, exercise, and smoking cessation for lifelong cardiovascular and pulmonary health.
These strategies aim to improve the patient’s functional capacity, enhance quality of life, and reduce the risk of future heart or lung complications through a holistic and tailored approach.
CHIROPRACTIC & OSTEOPATHY TECHNIQUES
Chiropractic techniques focus primarily on the spine and nervous system. Common methods include spinal manipulation (adjustments) to realign the spine, soft tissue therapy to relax muscles, and trigger point therapy to relieve muscle tension. Chiropractors aim to improve joint mobility, alleviate nerve pressure, and reduce pain, often treating back pain, neck pain, and headaches.
Osteopathy takes a more holistic approach, targeting the entire body. Techniques like osteopathic manipulative treatment (OMT), myofascial release, and cranial osteopathy focus on improving the body’s structure and function by addressing imbalances in joints, muscles, and connective tissues. Osteopaths use gentle manual therapy to improve circulation, reduce pain, and enhance overall body function.
By combining both disciplines, a comprehensive, non-invasive solution for musculoskeletal pain and improved mobility is provided, benefiting conditions such as chronic pain, joint stiffness, and muscle imbalances.
FITNESS CONSULTATION
A fitness consultation with a physiotherapist focuses on creating a personalized exercise plan based on your physical condition, goals, and any underlying health concerns. During the consultation, the physiotherapist assesses your mobility, strength, posture, and any existing injuries. They consider factors like fitness level, flexibility, balance, and movement patterns to design a safe, effective workout routine.
Physiotherapists emphasize injury prevention and often recommend exercises that improve strength, endurance, flexibility, and overall functionality. This approach helps in rehabilitating injuries, enhancing physical performance, and maintaining long-term health. It’s ideal for individuals recovering from injury, starting a fitness journey, or seeking expert guidance on maintaining optimal body function.
EXERCISE PRESCRIPTION
Exercise prescription by a physiotherapist involves designing a customized exercise program tailored to your specific needs, goals, and physical abilities. After a thorough assessment of your strength, mobility, flexibility, balance, and any existing injuries, the physiotherapist creates a plan to address these areas while ensuring safety and effectiveness.
The exercises prescribed are aimed at improving muscle strength, endurance, cardiovascular fitness, flexibility, and functional movement. They also focus on preventing injury, enhancing recovery, and promoting long-term physical health. Exercise prescription is ideal for rehabilitation, sports performance, weight management, or general fitness, ensuring you progress safely toward your fitness goals.
PREHAB
Prehab, or prehabilitation, is a proactive approach to improving physical fitness and strength before undergoing surgery, or to prevent injuries during physical activity. The goal of prehab is to optimize muscle strength, joint mobility, balance, and overall function in preparation for surgery or intense physical demands.
By starting a targeted exercise program early, prehab helps improve recovery time, reduce complications, and ensure better post-surgery outcomes. It also helps individuals prevent injuries by addressing muscle imbalances, improving flexibility, and strengthening areas vulnerable to strain. Prehab is commonly recommended before orthopedic surgeries like joint replacements and for athletes to minimize the risk of injury during their training.
VESTIBULAR REHABILITATION
Vestibular rehabilitation is a specialized form of therapy designed to address dizziness, vertigo, balance disorders, and other symptoms caused by issues in the vestibular system, which includes parts of the inner ear and brain that control balance and eye movements. This therapy is typically prescribed for conditions like vestibular neuritis, benign paroxysmal positional vertigo (BPPV), Meniere’s disease, or after an injury affecting the inner ear.
The goal of vestibular rehabilitation is to reduce dizziness, improve balance, and enhance overall stability through specific exercises. These exercises are focused on improving gaze stability, posture, and spatial orientation. Patients may be guided through activities that help retrain the brain to adapt to vestibular changes, enhancing coordination, and reducing the risk of falls. It's highly effective in restoring normal function for individuals experiencing chronic dizziness and balance issues.
PAEDIATRIC PHYSIOTHERAPY
Pediatric physiotherapy is a specialized branch of physiotherapy that focuses on helping children from infancy through adolescence achieve their optimal physical development. It addresses a wide range of conditions, including developmental delays, neurological disorders (like cerebral palsy), musculoskeletal issues, genetic conditions, and injuries.
Pediatric physiotherapists work to improve motor skills, strength, balance, coordination, and flexibility in children. Therapy sessions are designed to be engaging and fun, incorporating play-based activities that help children develop their physical abilities in a comfortable and supportive environment.
The goal is to enhance a child's ability to participate in daily activities, improve mobility and independence, and promote healthy physical development. Pediatric physiotherapy also focuses on educating families to ensure children continue to progress at home and in their daily routines.
GERIATRIC PHYSIOTHERAPY
Geriatric physiotherapy is a specialized form of physiotherapy that focuses on the unique needs of older adults. It aims to help seniors maintain or improve mobility, strength, balance, flexibility, and overall physical function. Geriatric physiotherapists work with individuals who may be dealing with conditions related to aging, such as arthritis, osteoporosis, joint replacements, and neurological disorders like Parkinson’s disease or stroke.
The goal of geriatric physiotherapy is to improve quality of life by reducing pain, increasing independence, and preventing falls or injuries. It includes strengthening exercises, balance training, mobility exercises, and postural corrections, all tailored to the specific needs of the elderly. Additionally, it often involves education on maintaining physical health, adapting to physical changes, and maximizing functional abilities to promote a healthier, more active lifestyle for older adults.

Approach toward the patient’s problem and customisation of the therapy makes the treatment more effective . Roy Physiocare can be blindly banked upon for any neuro and ortho therapy.
Sabyasachi Chanda

Akash is a very talented and hard working physio indeed who strives to solve the patient's problems with care and dedication unlike some other physios who like to drag the treatment unnecessarily to try and make money. Instead he retains patients by delivering outcome and relief. Keep up the positive attitude and you will go far 👍
Seassan Hashmi

★★★★★
★★★★★
Sales manager, Asia Pacific Region, Wipro
Founder & CEO, Force Ten Technologies
Take a glance at what patients say about us
Roy Physiocare
Your A to Z Physiotherapy Solution
© 2026 Roy Physiocare. All rights reserved.


Call us:
